Summary
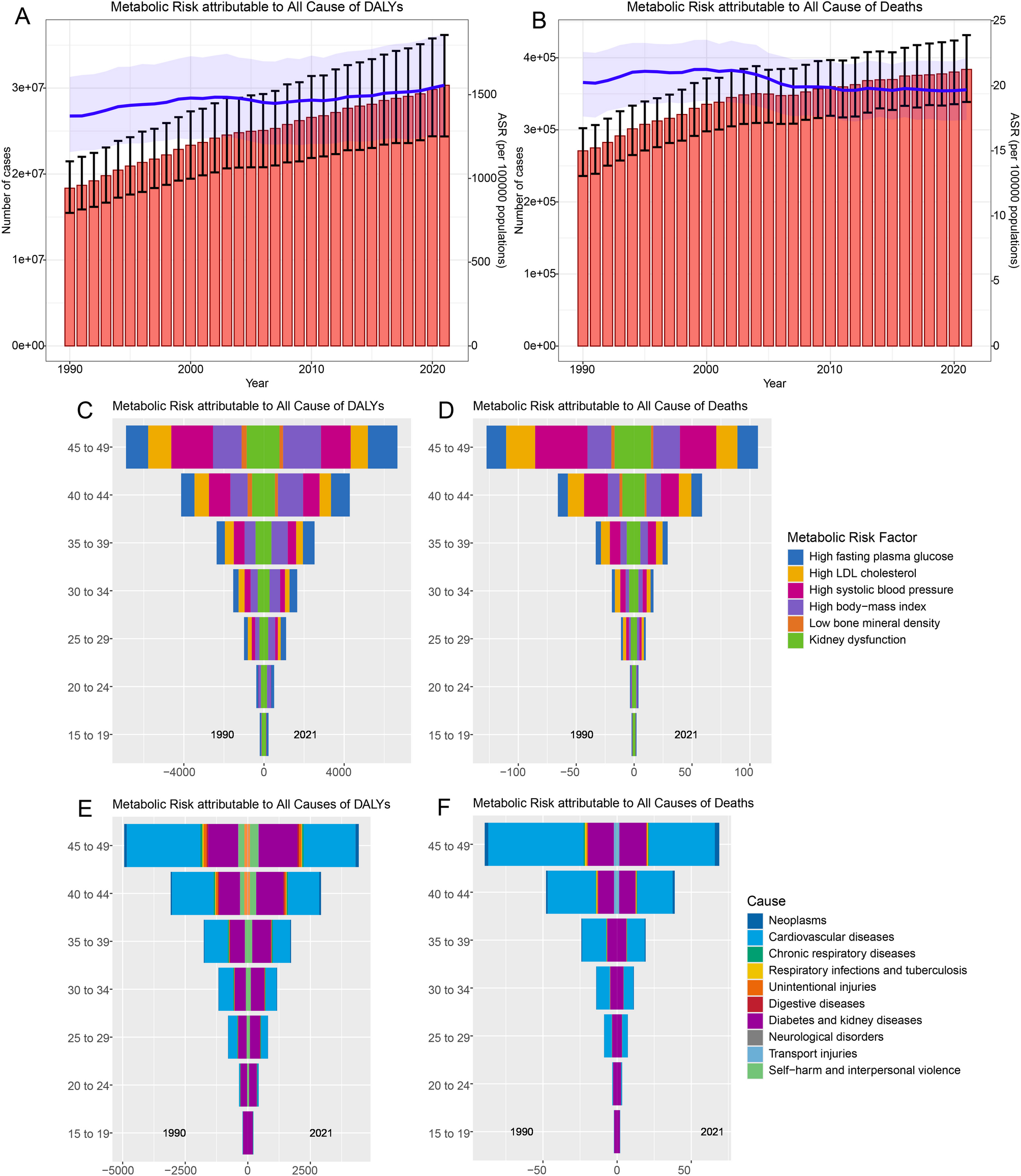
This study provides a comprehensive analysis of the global burden of metabolic risk factors among women of reproductive age (1549 years) from 1990 to 2021, utilizing data from the GBD 2021 study. The findings reveal a significant increase in DALYs attributable to metabolic disorders in this demogra…
Source: BMC Womens Health

AI News Q&A (Free Content)
Q1: What are the primary metabolic risk factors contributing to disease burden among women of reproductive age?
A1: The primary metabolic risk factors contributing to disease burden among women of reproductive age include high body mass index (BMI) and high fasting plasma glucose. These factors have been identified as leading contributors to the increase in disability-adjusted life years (DALYs) among this demographic, emphasizing the significant impact of metabolic disorders on women's health globally.
Q2: How has the global burden of metabolic disorders among women of reproductive age changed from 1990 to 2021?
A2: From 1990 to 2021, there has been a significant increase in the global burden of metabolic disorders among women of reproductive age. In 2021, metabolic risks accounted for approximately 30.3 million DALYs among women aged 15–49 years worldwide, translating to an age-standardized rate (ASR) of 1,556.2 DALYs per 100,000 population. This increase underscores the urgent need for targeted health interventions to address these risks.
Q3: What regions are most affected by metabolic diseases, and how do these burdens differ globally?
A3: The highest absolute burden of metabolic diseases is found in populous countries such as India, China, and the United States. In contrast, the highest relative burden is concentrated in Oceania Island states. This variation highlights significant regional disparities in the prevalence and impact of metabolic disorders globally.
Q4: What are some recent scholarly findings on metabolic syndrome in women from the Study of Women's Health Across the Nation (SWAN)?
A4: Recent findings from the SWAN study indicate that metabolic syndrome among middle-aged women is influenced by various factors identified through Bayesian machine learning techniques. The RR-BART method used in this research has successfully identified predictors for metabolic syndrome that were less commonly recognized previously, offering new insights into the biological underpinnings of this condition.
Q5: How do socioeconomic factors like income and education affect fertility rates among women of reproductive age?
A5: Socioeconomic factors such as income and education significantly affect fertility rates among women of reproductive age. Studies show a negative relationship between income and fertility for women aged 20–29, suggesting that having children is perceived as an opportunity cost. Additionally, higher education levels are associated with reduced teenage fertility, emphasizing the role of socioeconomic conditions in reproductive decisions.
Q6: What are the implications of the findings from the Global Burden of Disease 2021 study for public health policy?
A6: The Global Burden of Disease 2021 study highlights the need for comprehensive public health policies targeting metabolic risk factors. Interventions focusing on improving behavioral and metabolic risks, such as managing high blood sugar and BMI, could significantly reduce the global disease burden. Policymakers are urged to prioritize these areas to enhance health outcomes for women of reproductive age.
Q7: What are the potential public health interventions suggested for reducing the burden of metabolic disorders globally?
A7: Potential public health interventions include promoting healthier lifestyles through improved diet and physical activity, managing high blood pressure and glucose levels, and reducing smoking rates. Such measures could lead to a substantial decrease in DALYs globally, as evidenced by scenarios where behavioral and metabolic risks are mitigated.